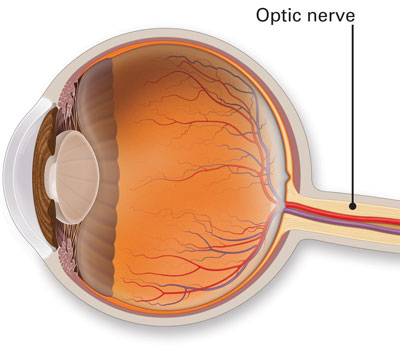
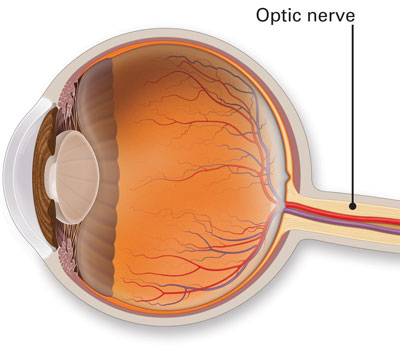
The Optic Nerve carries electrical impulses from the eye to the brain and enables us to see. Neuro Ophthalmology is the subspecialty that deals with disorders of the optic nerve. Common disorders include optic neuritis (inflammation and swelling of the optic nerve), Ischemic Optic neuropathies (Decreased blood supply to the optic nerve) and Traumatic optic neuropathy. Diagnosis of these disorders requires electrophysiological tests such as VEP/ERG and EOG.
(For further information please refer to frequently asked questions)
Team for Neuro - Ophthalmology
Frequently Asked Questions
Neuro-ophthalmology is an ophthalmic subspecialty that addresses the relationship between the eye and the brain, specifically disorders of the optic nerve, orbit, and brain, associated with visual symptoms. Neuro-ophthalmologists provide comprehensive clinical care to a broad spectrum of patients with visual disturbance from optic nerve diseases, central nervous system disorders, ocular motility dysfunction, and pupillary abnormalities. Over 50 percent of all intracranial lesions involve the visual or oculomotor pathways. Shroff Eye Centre offers you a dedicated Neuro-Ophthalmology Service for the diagnosis and treatment of these neuro-ophthalmic disorders.
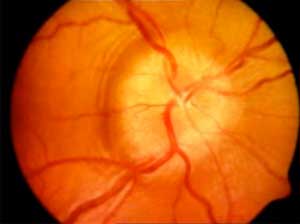
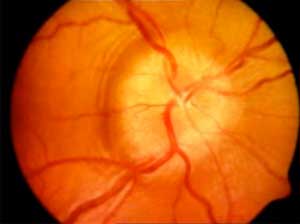
This is the most common cause of sudden decreased vision in patients older than 40 years. We do not see with our eyes. We see with part of our brain that is capable of interpreting visual signals sent back from the eyes. This is located at the back of our head (the occipital lobes). Information is transmitted from the eyes to the brain via the optic nerves. These nerves are composed of the long tube extensions (axons) of cells (ganglion cells) located within the inner lining of the eye (the retina) that exit the back of the eye at the optic disc. Each of the optic nerves receives blood supply from branches of the ophthalmic artery within each eye socket. The optic disc has a unique blood supply (the posterior ciliary arteries).
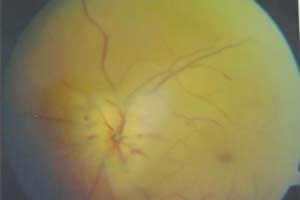
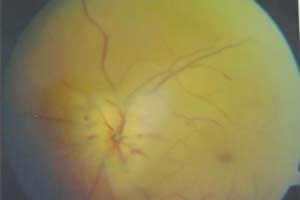
Loss of blood supply within the posterior ciliary arteries deprives the optic nerve tissue of oxygen and results in damage to part or all of the optic nerve. This is a small "stroke" in the optic nerve. It is painless. Patients may become aware of decreased vision or difficulty seeing above or below the center of gaze. Loss of the blood supply results in swelling of the optic disc, often associated with hemorrhages. The hemorrhages and swelling will go away leading to the development of a pale disc (optic atrophy). As the swelling resolves, some of the axons will be permanently lost. We do know that this happens more often in patients who are born with small optic discs. These episodes may occur when there is a sudden drop in blood pressure (following an operation or associated with blood loss after an accident). Patients who smoke, or who have diabetes or high blood pressure, may be at higher risk for AION.
Know More...
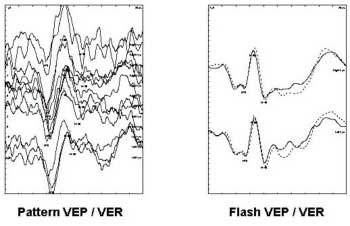
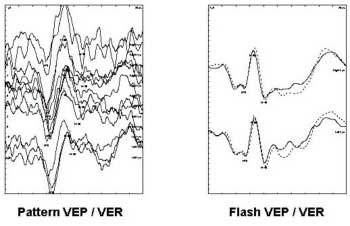
VEP measures the electrical responses generated at visual cortex in response to a visual stimulus with the help of electrodes. It is helpful in:
Optic nerve disease
Cortical Blindness
Visual assessment in preschool children
Malingerers
Amblyopia
A special type of flash VEP is helpful in cases with media opacity as a rough method to indicate that light is perceived.
Know More...
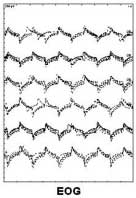
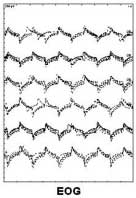
This test examines the function of the retinal pigment epithelial cells (RPE). When this layer is healthy a standing potential is established between the front and the back of the eye that responds to change in background illumination. The standing potential can be measured by measuring the voltage induced across a pair of electrodes put around the eye as the eye looks from side to side. The test is most useful for a hereditary retinal degeneration called Best's disease.
Know More...
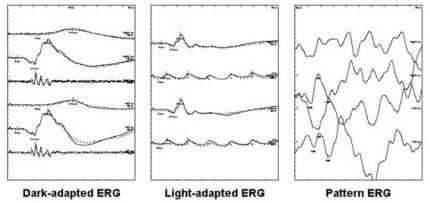
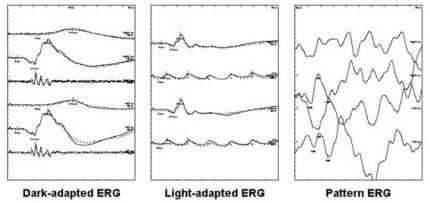
The ERG is the mass electrical response of retina in response to a bright flash of light and is recorded using corneal electrodes. It reflects the function of the retinal photoreceptors (rods and cones) and the inner nuclear layers of retina. It is often useful for:- " Diagnosing and predicting outcome of inherited retinal degeneration.
Early diagnosis of retinal degeneration in children with family history of inherited retinal degeneration.
Differentiating types of retinal degeneration (cone-rod, rod-cone type).
Prognosticating high risk characteristics in cases of central retinal vein occlusion.
Unexplained vision loss
Know More...
Ocular Electrophysiology (Electrodiagnostics)
Electrophysiological examination provides objective information in relation to the function of the visual pathway helping in diagnosis and management of the patient. The main tests are Electro-retinogram (ERG), Visual evoked potential (VEP) and Electro-oculogram (EOG). These are used to locate the site of disease whether in the retina, optic nerve or brain, and to decide the extent of disease. They help to decide the potential for visual recovery and appropriate treatment. Light stimulus produces electrical waveforms and the machine picks up the waveforms and displays it on a monitor and as printout. Shroff Eye Centre offers you a dedicated Ocular Electrodiagnostics Service for the diagnosis of disorders related to the visual pathway.
The following tests are available:
The Electro-Retinogram (ERG)
The Visual Evoked Potential (VEP)
The Electro-oculogram (EOG)

Know More...
Steroid therapy may be effective in halting the inflammatory phase of thyroid orbitopathy and partially shrinking the muscle swelling. Steroid side effects are very common with continued treatment. If there are still problems with eye movements (double vision), exposure problems (irritation and foreign body sensation), or decreased vision then surgery should be considered.
Know More...
In patients with mild involvement, irritation and foreign body sensation may improve with artificial tears and the use of lubricating ointment at night. If the lids are not closing completely, they may be taped closed at night. With more severe corneal problems, lid surgery to help partially close the lids or to raise the lower lids may be necessary. In severe retraction of the upper or lower lid, surgery to reduce the effects of the lid retractors, either without or with spacer placement (such as a piece of tissue removed from the roof of the mouth) can help the lids to close. Smoking may worsen symptoms and should be discontinued.
There is no medicine that improves the ability of muscles to move (and thus relieves double vision). Covering one eye immediately relieves double vision. It may be possible to optically realign eyes with the use of prisms either applied to glasses or ground into the lens although this may not be effective until things stabilize. When double vision cannot be corrected with prisms, eye muscle surgery may be necessary. Often multiple muscle operations are necessary. It is sometimes not possible to completely remove double vision, but the goal is to remove double vision looking straight ahead and in reading position, as these are the most important directions of sight.
Fortunately, optic nerve problems resulting in decreased vision are uncommon. When it occurs, treatment is aimed at shrinking the muscles, usually by the use of high dose steroids (prednisone). For those patients who will not tolerate steroids radiation therapy may be of benefit. If the muscles cannot be made small enough to relieve the compression of the optic nerve (resulting in decreased visual acuity) then the orbit can be made larger. This is usually done surgically by removing one or more of the bony walls of the orbit. Since the optic nerve is usually compressed at the very back of the orbit, removing the posterior medial wall of the orbit is most critical. This may be done directly (through the soft tissues or skin around the eye), through the sinus under the eye, or through the nose. To further reduce the eye bulge the floor, lateral wall, or even the roof of the orbit may be removed. One of the problems with surgical decompression is that this often affects eye movements, thus changing the pattern of double vision (if it already exists) or potentially producing double vision in those patients who don't have it before surgery.
Know More...
Thyroid orbitopathy, like other autoimmune diseases, often comes and goes on its own. There is frequently only one acute inflammatory episode but unfortunately the effects may persist for years or even permanently. Although there may be some reduction of the prominence of the globe, eye movements will often not return to normal. Lid position will also likely remain elevated, possibly with persistent problems with closure.
Know More...
This is detected by carefully checking vision, pupillary reactivity, visual fields, and the appearance of the optic nerve head. Most frequently this makes the thyroid gland over produce thyroid hormone that in turn can lead to tremors, shakes, weight loss, rapid heart beat or palpitations, nervousness, and sensitivity to heat. Less commonly the attack on the thyroid gland leads to low thyroid production or even normal thyroid levels. We may see antibodies in your blood that can be identified as attacking thyroid tissue.
Know More...
With muscle enlargement the globe (eyeball) is pushed forward leading to the characteristic "stare." In addition, the muscles become stiff and the upper lid tends to retract, pulling away from the colored portion of the eye. The eyes may become red due to difficulty closing as well as increased prominence of the blood vessels. This often results in double vision with one image seen on top of the other. If the muscles get large enough, they may press on the optic nerve causing damage to the nerve.
This dysfunction within the optic nerve, which transmits information from the eye to the brain, results in decreased vision. This, fortunately, occurs only in about 5% of the patients with thyroid orbitopathy and may be reversible if the pressure on the optic nerve is relieved.
Know More...
This is an autoimmune condition where your body's immune system is producing factors that stimulate enlargement of the muscles that move the eye. This can result in bulging of the eyes, retraction of the lids, double vision, decreased vision, and ocular irritation. This is often associated with abnormalities in thyroid gland function (either too much thyroid (Graves' disease) or too little). The eye findings of thyroid orbitopathy may be independent of treatment of your thyroid abnormalities and may not resolve in spite of the fact that the thyroid is now "controlled." These symptoms may be present even if your thyroid has no apparent problems.

Know More...
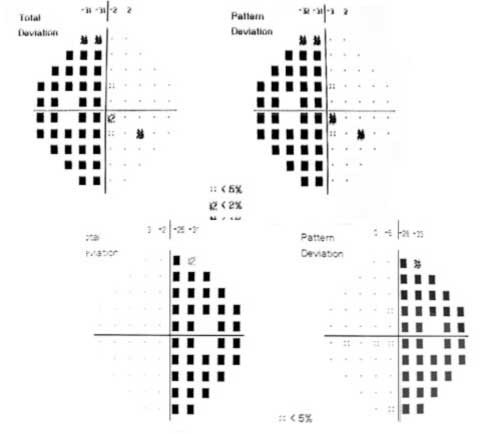
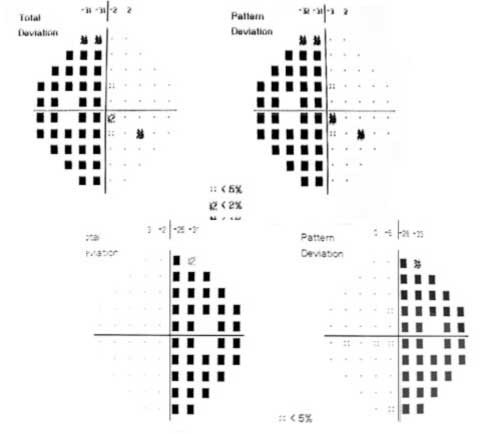
Reduction in CSF production or increase in its outflow may reduce intracranial pressure. Weight reduction programs (in overweight patients) may be effective. Continuous drainage may be surgically accomplished by placing a catheter between the spinal canal and the abdomen (lumbo-peritoneal shunt). In patients with worsening visual fields or decrease in central acuity, who do not have severe headaches, an optic nerve sheath fenestration may protect the optic nerve from further damage. A small hole or multiple slits are placed in the optic nerve sheath just behind the eye using an operating microscope.
Know More...
The patient requires a MRI scan. The diagnosis also requires a spinal tap. This will document elevated pressure inside your head and make sure there are no other abnormalities in the CSF. The finding of abnormal cells, inflammatory cells, or elevated protein may indicate a previous infectious, inflammatory, or tumor related cause of elevated intracranial pressure. In rare cases, an angiogram, where a catheter is placed in the arteries and veins going to the head, may be necessary to exclude an abnormality of the blood vessels. To determine whether there is further damage to the optic nerve acuity and visual field testing is necessary.
Know More...
The most common symptoms of high intracranial pressure are headache and visual loss. The headache may be located anywhere; frequently in the back of the neck. It is usually steady but may be pounding. It may be very severe, and unlike migraine, it may awaken the patient in the middle of the night. It also may worsen with bending or stooping. The optic nerve swelling may eventually lead to loss of vision seen as dimming, blurring or graying of vision. Patients may be aware of difficulty seeing to the side. Frequently patients notice visual disturbance lasting for a few seconds (often associated with bending or stooping). High pressure may cause damage to the nerves that move the eyes resulting in double vision. Patients may also be aware of a rushing noise in their ears. Nausea and vomiting may occur if the pressure is high and especially with a severe headache. Peripheral vision (detected on visual field testing) is usually abnormal and is one of the most important means of judging both the necessity for and effectiveness of treatment.
Know More...
This is a condition in which high pressure inside your head can cause problems with vision and headache. In papilledema cerebrospinal fluid outflow is blocked. The pressure is transmitted to the back of the eye via the optic nerve sheath (surrounding each of the optic nerves) producing the swelling seen at the disc (papilledema).
Know More...
In patients with visual loss due to compression of the optic nerve or chiasm by a pituitary tumor the chance of visual improvement is best predicted by the duration of the damage. The presence of changes in the back of the eye (optic atrophy) may suggest long duration. Surgery also can result in rapid relief of compression.
Know More...
When the patient is symptomatic, some form of treatment is usually indicated. The most common approach is surgery usually performed through the nose (or up under the lip). Occasionally (especially when the tumor is larger or extending to the side) a surgical approach may be best through a scalp incision. With large tumors, some tumor cells are almost always left behind following surgery. Additional treatment may be needed. This may include repeat surgery or radiation therapy. It is very important that hormone levels be checked periodically and replaced as necessary. It is also important to follow vision, visual fields, and imaging studies (MRI scan) to make sure that there is no re-growth of the tumor. These should probably be checked at least once every one to two years.

Know More...
Pituitary tumors are usually suspected based on endocrine changes but are confirmed with imaging studies. A CT scan can reveal a pituitary tumor and may be especially sensitive to hemorrhage. MRI scanning may be more sensitive and better define the relationship of the tumor to the optic nerves and surrounding structures. Blood studies to check pituitary function are essential. Other lesions around the sella and pituitary may produce similar symptoms and may be confused with a pituitary tumor. These include meningiomas, craniopharyngiomas, germ cell tumors, and aneurysms.
Know More...
Patients with pituitary tumors often have no symptoms at all. Occasionally these tumors may produce headaches. Head pain may be sudden and severe if there is a bleed into the tumor. Endocrine symptoms are most common including alterations in menstruation, lactation (milk from the breast), impotence, or loss of sex drive. Less commonly, tumors may produce growth hormone causing gigantism in young patients or enlargement of hands, feet, and facial features (acromegaly) in older patients. The most common of these symptoms is due to compression of the optic nerves or chiasm. Patients with involvement of one optic nerve may notice dim, dark, or blurred vision. If the chiasm is affected, vision will be lost off to the outside in both eyes.
Know More...
Pituitary tumors are benign (non-cancerous) overgrowth of cells that make up the pituitary gland (the master gland that regulates other glands in the body). Tumors that grow large enough to produce symptoms are less common but still are one of the most common tumors occurring within the head. These tumors may often be present for years without diagnosis or even symptoms.
The optic nerves coming from each eye meet just above the pituitary gland in the optic chiasm. An abnormal growth of cells within the pituitary gland may produce an excess of signal to the other endocrine glands leading to overproduction of thyroid, cortisone, or sex hormones. If the pituitary tumor extends out of the sella it may produce symptoms due to compression of surrounding structures including the optic nerves, chiasm, and cranial nerves in the cavernous sinus (controlling eye movement and facial sensation).
Know More...
Multiple sclerosis (MS) is a disease process where the body's immune system attacks multiple areas in multiple episodes. An episode of optic neuritis may be the first indication of multiple sclerosis. With a single episode, without other evidence of involvement, we usually cannot make the diagnosis at that time. An MRI scan may be helpful in dividing those patients into high and low risks. Finding evidence of other areas of inflammation on MRI scanning suggests you may be at higher risk for recurrent episodes and thus MS.

Know More...
Patients treated with oral (pills) steroids seem to have a higher chance of recurrent episodes. Therefore, steroid pills alone are not recommended as treatment. Patients who were treated with intravenous (given by needle) steroids did have a slightly more rapid recovery of their vision, although the final visual outcome was not better than in those who were not treated. Thus, IV steroids can be recommended for patients with severe involvement or involvement of both eyes.
Know More...
The pain will go away, usually in a few days. The vision problems will improve in the majority (92%) of patients. There are rare patients who have continued progressive loss of vision. Frequently colors look different or "washed out." Visual recovery usually takes place over a period of weeks to months, although both earlier and later improvement is possible. Optic neuritis can recur involving the same eye, the other eye or other parts of the central nervous system (brain and spinal cord). This may result in recurrent episodes of decreased or loss of vision or problems with weakness, numbness or other signs of brain involvement. An MRI scan can give us a rough guess as to the likelihood of recurrence. Other testing techniques include visual evoked potentials (a test where you are shown a checkerboard of light and signals are recorded from electrodes on your scalp) that can show a delay in conduction due to the damage to the myelin.
Know More...
A few patients with optic neuritis have swelling of the optic disc (the beginning of the optic nerve) at the back of the eye. This is referred to as papillitis. One sign usually detected by your eye doctor is the presence of an afferent pupillary defect. This indicates that there is less light being sensed by the affected eye than the opposite eye. This is found by swinging a bright light back and forth between your two eyes while observing how your pupil reacts.
Know More...
The most common symptom of optic neuritis is sudden decrease in vision. In mild cases, it may look like "the contrast is turned down" or that colors appear "washed out." This may vary and, not infrequently, will progress from the time it is first noticed. The second most common symptom associated with optic neuritis is discomfort in or around the eye often made worse by movement of the eye.
Know More...
This is the most common cause of sudden visual loss in a young patient. It is often associated with discomfort in or around the eye, particularly with eye movement. The optic nerve fibers are coated with myelin to help them conduct the electrical signals back to your brain. In the most common form of optic neuritis, the optic nerve has been attacked by the body's overactive immune systemA viral infection that may have occurred years, or even decades, earlier may have set the stage for an acute episode of optic neuritis. The inflammation associated with optic neuritis can result in discomfort (particularly with movement of the eye).
Know More...
Since we expect the double vision to clear up on its own any treatment will hopefully be necessary for only a few weeks or months. The easiest way to get rid of the double vision is to wear a patch. Alternatively one lens of your glasses may be fogged using frosted cellophane tape on the inside.
Know More...
There is no known means of accelerating the natural recovery characteristic of microvascular cranial nerve palsy. It is important to make sure that blood pressure and blood sugar are adequately controlled. The double vision may be treated acutely with patching either eye. It is very important that patients report any new symptoms or failure of the double vision to resolve.
Know More...
While it is possible for multiple cranial nerve palsies to have a microvascular cause all patients with more than a single nerve palsy or with other neurologic findings must have a work up (neurologic examination and imaging study) before the diagnosis is accepted. If the cranial nerve palsy fails to resolve completely over 3 months additional work-up is indicated. All patients with presumed microvascular cranial nerve palsies should have their blood pressure and blood sugar checked to make sure they do not have diabetes or hypertension. Additional work up such as CT or MRI scans or even an angiogram to rule out an aneurysm may be necessary.
Know More...
Dysfunction of one cranial nerve will produce weakness in one or more muscles. If the eyes aren't moving together the patient will experience blurred or double vision. If only the VIth nerve (innervating the lateral rectus) is affected the double vision will be side to side. If the IIIrd or IVth nerve is affected there will most commonly be some vertical ("one on top of the other") double vision. This will vary depending on the direction of gaze.
Know More...
This is one of the most common causes of acute double vision in the older population. It occurs more often in patients with diabetes and high blood pressure. These will get better and essentially always resolve without leaving any double vision. However, compressive masses, infections, inflammation and injury can also cause cranial nerve palsy. The eyes are moved by 6 extra-ocular muscles. Four of these are rectus muscles (superior, inferior, medial, and lateral) that attach to the front part of the eye (just behind the iris, the colored portion of the eye). Two muscles (the superior and inferior oblique) attach to the back of the eye. These 6 muscles receive their signals from 3 cranial nerves (the IIIrd [oculomotor], IVth [trochlear], and VIth [abducens]). These nerves originate in the brain stem (at the base of the brain) and enter the eye socket through a fissure in the bone of the skull behind the eye.
Pressure on or Interruption of the blood supply to one of the cranial nerves causes it not to work. If there is interruption of signal to the VIth nerve (which innervates the lateral rectus muscle) the affected eye will not be able to move to the outside. The patient will be aware of side-to-side double vision that will be worse (further separation) when the patient looks towards the affected sideWhen the IIIrd nerve (which goes to multiple muscles) is involved the eye may be limited in up, down, and gaze toward the nose. The patient is usually aware of combined vertical and side to side double vision although there may be no double vision at all since the lid droops and may block the second image. The nerves are not permanently injured and over a period of 6 to 12 weeks the function should recover.

Know More...
Unfortunately, at this time there is no proven treatment for patients with AION. It has been suggested that aspirin (regular size or baby aspirin once a day) may decrease the chance of an episode in the opposite eye. It is important that the blood pressure be followed by your doctor (elevated pressure increases risk). On the other hand it is important that there be no sudden drop in blood pressure (overly aggressive treatment). Smoking should be stopped.
Know More...
Most patients with ischemic optic neuropathy will have relatively stable vision. A recent study suggests that 40% of patients may expect to have some improvement in central vision. A very small number of patients can have worsening of vision. In patients who have had AION there is a possibility of this happening in the other eye. Fortunately, this is not common (approximately 20% chance). Probably the best news is that it is very rare for a second episode of ischemic optic neuropathy to occur in the same eye.
Know More...
Most patients with AION notice a sudden painless disturbance in their vision. Because of the decreased optic nerve function, however, the pupils may not react as well when light is directed into the affected eye. Swinging a flashlight between the two eyes will then show an "afferent pupillary defect." Visual field testing can identify the area of optic nerve dysfunction. Blood pressure should be checked and if there are any unusual features other blood studies may be done. In elderly patients a blood test (sedimentation rate or c-reactive protein) can help assess the risk of giant cell arteritis.
Know More...
This is the most common cause of sudden decreased vision in patients older than 40 years. We do not see with our eyes. We see with part of our brain that is capable of interpreting visual signals sent back from the eyes. This is located at the back of our head (the occipital lobes). Information is transmitted from the eyes to the brain via the optic nerves. These nerves are composed of the long tube extensions (axons) of cells (ganglion cells) located within the inner lining of the eye (the retina) that exit the back of the eye at the optic disc. Each of the optic nerves receives blood supply from branches of the ophthalmic artery within each eye socket. The optic disc has a unique blood supply (the posterior ciliary arteries).
Loss of blood supply within the posterior ciliary arteries deprives the optic nerve tissue of oxygen and results in damage to part or all of the optic nerve. This is a small "stroke" in the optic nerve. It is painless. Patients may become aware of decreased vision or difficulty seeing above or below the center of gaze. Loss of the blood supply results in swelling of the optic disc, often associated with hemorrhages. The hemorrhages and swelling will go away leading to the development of a pale disc (optic atrophy). As the swelling resolves, some of the axons will be permanently lost. We do know that this happens more often in patients who are born with small optic discs. These episodes may occur when there is a sudden drop in blood pressure (following an operation or associated with blood loss after an accident). Patients who smoke, or who have diabetes or high blood pressure, may be at higher risk for AION.
Know More...
A few of the most common neuro-ophthalmic conditions are optic neuritis, ischemic optic neuropathy, compressive optic neuropathy (including pituitary tumors), papilledema, inflammatory and infectious optic neuropathies, cerebrovascular disorder involving vision, tumors involving vision, blephrospasm & hemifacial spasm, thyroid eye disease, myasthenia gravis, ocular motor disorders (including cranial nerve palsies), pupillary abnormalities, hereditary optic neuropathies and patients who have unexplained visual loss.
Know More...
Symptoms that are more common in neuro-ophthalmic disease include visual loss, visual disturbance, diplopia, unequal pupils and eyelid and facial spasms.
Know More...
 Dr. Varshini Shanker
Dr. Varshini Shanker







 Call us
Call us Email us
Email us