Your Eyes, Our Passion
How successful is corneal transplantation?
How successful is corneal transplantation?
Corneal transplantation restores vision only in eyes that have been partially blinded by corneal disease. If a person is blinded by glaucoma, a detached retina, or degenerative change and the retina has been damaged or destroyed, nothing can restore lost sight.
In favorable subjects, the rate of success of corneal transplantation may be as high as 90%, with good final visual acuity with glasses. In unfavorable subjects, the rate of success may be around 10 to 20%. Each patient is evaluated individually before definite results can be predicted. The most important factors in determining the final results are:
• Basic corneal disease (some types of corneal disease respond better to corneal transplantation than others).
• State of the donor’s cornea.
• Surgical technique and skill.
• Healing ability of the recipient cornea.
• Sensitivity reactions between donor and recipient cornea may lead to transplant rejection.
• Presence of concurrent eye diseases like glaucoma, retinal diseases reduce the chances of good visual outcome
The advantages of lamellar keratoplasty (newer techniques) are better visual outcome, quicker rehabilitation and lower rates of transplant rejection.
ADVANCES & NEW DEVELOPMENTS IN CORNEAL TRANSPLANTATION TECHNIQUES
Selective Keratoplasty:
Some of the complications after transplant are due to transplantation of tissues that were not required for the correction of the primary disease per se. Thus, fewer complications may be expected when only the diseased corneal layer is replaced with donor tissue. Today depending on the extent, location and type of the corneal disorder, we can selectively transplant either the front part (Anterior Lamellar Keratoplasty), or the back portion (Endothelial Lamellar Keratoplasty).
Endothelial Keratoplasty:
In conventional corneal transplant surgery (Penetrating Keratoplasty), the surgeon removes the window of cloudy tissue from patient’s cornea and replaces it with a clear corneal tissue. This transplanted cornea is held in its place with multiple tiny stitches. To allow healing, these stitches must remain in their place for at least 6 months. These stitches induce an irregular spectacle number (irregular astigmatism) in the eye and it takes long to get a clear vision.
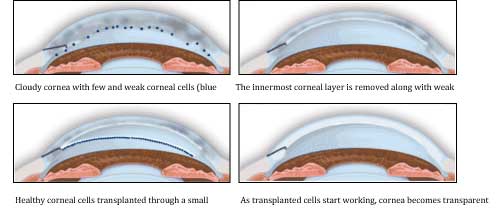
DSEK and DSAEK is a selective keratoplasty in which only the diseased endothelial layer of cornea is replaced by a healthy donor tissue. The procedure requires precision guided dissection of donor tissue to retrieve only the innermost layers of cornea. This can be accomplished with an automated micro-keratome or by Femtosecond Laser (IntraLaseTM). As less tissue is transplanted, lower rejection rates may be expected, esp. epithelial and stromal rejection. DSEK/DSAEK procedure requires less number of sutures, it is safer and visual recovery is faster compared to conventional penetrating corneal transplant.
What happens if the graft fails?
Graft failure can occur due to infection, rejection or glaucoma. Should the graft fail, it can be replaced by a repeat corneal transplantation.
Corneal graft rejection:
Patient’s immune system can identify the transplanted cornea and mount a reaction against it. As a natural phenomenon, any organ transplant carries a risk of rejection. A severe rejection episode can cause irreversible loss of function and graft fails. However, recognizing early warning signs of rejection and a regular follow-up can prevent graft failure due to rejection. This is why a regular and long-term follow up is required after corneal transplant.
Corneal transplant is a human effort to match what nature has created. Many factors like graft rejection, infection, astigmatism and glaucoma limit the ultimate success of corneal grafting. Despite many limitations, corneal transplant is still the most successful story among all organ transplant procedures.
Endothelial Keratoplasty / Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK)
Introduction:
Corneal endothelium is the innermost layer of cornea. It comprises of a layer of endothelial cells lined by a thin transparent membrane (Descemet’s membrane). The endothelial cells maintain corneal transparency by pumping excessive water from the corneal tissue. Any injury to endothelial cells is permanent as theses cells can not divide and grow once damaged.
Corneal endothelial disorders like pseudophakic bullous keratopathy (clouding of cornea after cataract surgery) and Fuchs’ endothelial dystrophy (clouding of cornea as a result of inherent corneal disease) are one of the major indications of corneal transplantation. Ideally, the corneal endothelium is the only layer that requires transplantation in these conditions, thus making endothelial transplantation as the treatment of choice. However, still majority of these cases undergo full thickness penetrating keratoplasty, which is often complicated by high irregular astigmatism (cylindrical number), a weak host graft junction due to slow wound healing, suture related infections and corneal graft rejection. Many of these complications can be avoided by a sutureless selective corneal endothelial transplantation technique. Descemet Stripping Endothelial Keratoplasty (DSEK) and its variations like Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) and Femtosecond Laser assisted DSAEK are modifications of endothelial keratoplasty. The fixation mechanism is so effective that sutures are not required. The posterior transplant consists of the endothelium, DM, and a thin layer of posterior stroma. It stays apposed to posterior corneal surface due to the negative pressure induced by pumping action of the donor. This is further helped by the stickiness of the stromal interfaces which may contribute to fixation of the transplant. The advantages of leaving patients anterior cornea intact are obvious as listed in Table 1.
Table 1: Advantages of endothelial keratoplasty (DSEK / DSAEK)
1. Reduced postoperative astigmatism.
2. Stable tear film
3. Early visual rehabilitation
4. No epithelial and stromal rejection
5. No postoperative suture-loosening and infections.
Donor preparation:
The method for harvesting the endothelium is a meticulous process. The donor cornea with is placed on an artificial chamber and lamellar dissection is done at the depth of 350 microns with specially designed instruments. Use of an automated technique like a microkeratome has decreased the failure rates of donor preparation.
Artificial Anterior Chamber (AAC, Figure 1) linked to the Amadeus II microkeratome is an excellent tool to obtain the posterior donor lamella for DSAEK. Advantages of donor preparation with micro-keratome are listed in Table 2. At present, microkeratome assisted DSAEK remains the procedure of choice for endothelial disorders of cornea.
Figure 1: Amadeus microkeratome assembled with artificial anterior chamber (AAC)
Table 2: Advantages of automated (microkeratome assisted) donor preparation:
1. Predictable donor thickness
2. Faster, less traumatic
3. Less interface haze
4. Better visual outcome.
DSAEK technique:
A small corneal incision is made and recipient’s damaged endothelial cells are removed. The harvested donor tissue is then inserted into the recipient eye. Different techniques have been described for the graft insertion which include folding method, push in technique and more recent pull-in technique using a specially designed inserter (Busin glide) along with endothelial grasping forceps.
Busin glide and endothelial grasping forceps are 2 critical instruments required in DSAEK. Busin glide (Figure 2) is used to atraumatically insert the endothelial tissue through a clear corneal incision. It has a platform for placement of endothelial tissue and a funnel-shaped tapering tip which is apposed at the corneal incision to allow insertion of the endothelial tissue with the assistance of an ‘endothelial grasping forceps’ (Figure 3). This 23-gauge micro-incision end-grasping forceps gently grasps the edge of the endothelial tissue to facilitate the ‘pull through’ technique.
Figure 2: Busin glide
Figure 3: Endothelial grasping forceps
The donor lenticule is then secured at its position by an air bubble injected through a small incision. The pull-in technique is summarized in Figure 4.
Figure 4: Pull-in technique
DSAEK results:
We have been performing DSEK procedure in Shroff Eye Centre for the last 3 years and have moved on to automated donor dissection with Amadeus II micro-keratome with a 450 micron head. Now, with Busin glide and endothelial grasping forceps, the DSAEK procedure has become even more predictable and less traumatic.
DSAEK procedure provides best results when there is no stromal opacity and ocular surface is healthy (Figure 5). However, many patients with a longstanding endothelial disease develop superficial corneal scarring and vascularization due to recurrent episodes of infections. We have found that a combining specialized additional procedures like superficial keratectomy at the time of DSAEK procedure removes most of the superficial scarring provides gratifying visual outcomes (Figure 6). Later on, these patients can be treated with laser to further improve the vision.
To conclude, DSAEK not only provides a lower induced astigmatism and faster visual recovery but also reduces the risks of graft failures associated with a conventional full thickness corneal transplant.
Legends to figures:
Figure 5: DSEK. Fig 5a. A clear DSEK graft in a patient with Psedophakic bullous keratopathy. Fig 5b. A well apposed posterior lenticule without any interface haze. Fig 5c. Pentacam Scheimpflug image showing the DSEK graft lenticule well apposed to the posterior surface of recipient cornea.
Request a call back
I agree to recieve more information regarding services and offers at shroff eye center via SMS and Email
Disclaimer
This is not medical advice. Your ophthalmologist will help you decide which procedure and lens is best suited for your eyes. Every patient and eye is different and thus the experience for every patient is variable.
All product and company names are trademarks or registered trademarks of their respective holders. Use of them does not imply any affiliation or endorsement by them.

By being on the website, your personal data is being processed for communication with you and providing services. We use cookies to collect and analyse information on site performance, usage, enhancement of customer usability and improvising the website. We have put in place terms of use,
By clicking on accept you agree to all the policies mentioned above. You can read more about them by clicking on read more and accept them individually.








 Call us
Call us Email us
Email us


