Your Eyes, Our Passion
Age Related Macular Degeneration
Globally, Age-Related Macular Degeneration (AMD) is the third most common cause of ‘legal’ blindness (WHO 2002) whilst in most western countries it is by far the commonest cause of blindness. Macular degeneration usually manifests after 50 years of age. With the rapid rise in the geriatric age group, which is the at-risk group, the disorder could take epidemic proportions and become a major public health consideration. At Shroff Eye Centre, we have a dedicated team of Vitreo-Retinal specialists committed to providing you with the best possible care to protect your vision.
Definition of Age-Related Macular Degeneration
Age-Related Macular Degeneration (AMD) is a disease associated with aging, characterized by damage to the central part of the retina called macula. Before we talk about what can go wrong, it is important to understand how the eye works when it is working properly.
Dry Age-Related Macular Degeneration
It is the most common form found in 90% of patients. Dry AMD occurs when the macular tissues get thin and slowly lose function. The most common symptom of dry AMD is the blurred vision which causes difficulty in recognizing faces, increases the light requirement for reading and other tasks. Visual deterioration is slow but usually not profound. About 10-20% of people with dry AMD advance to the wet form.
Wet Age-Related Macular Degeneration
It is the less common but more aggressive form of AMD. If it is not treated it may get worse rapidly. Wet AMD is caused by the proliferation of abnormal blood vessels under the retina which may exude or leak out fluid, or bleed and ultimately lead to the formation of a scar under the retina. The various treatment options to stall progress to the wet form and to restrict vision loss will be discussed.
Symptoms of Age-Related Macular Degeneration
- Diminution of vision in an important symptom of macular degeneration. This lack of ability to see objects clearly affects one’s ability to read, drive and see details.
- Straight lines appear crooked or wavy.
- A dark area appears in the center of vision e.g. words in the central part of the page look smudged.

Having one or more of these symptoms may not necessarily mean that one has AMD and it warrants an immediate eye check up (early detection is important).
Risk Factors for Age-Related Macular Degeneration
Age – is the greatest risk factor. Although AMD can occur during middle age, studies show that people over 60 years of age are at great risk. The risk increases with increasing age.
Family History of AMD increases the risk.
Race – White populations are more predisposed to suffer vision loss from neovascular AMD than Asian or African populations.
Smoking has a definite correlation
History of hypertension, heart disease, or lung infection adds to risk.

Detection of Age-Related Macular Degeneration
Early detection is of paramount importance as smaller lesions have a better recovery and chance of maintaining reading vision than advanced cases with larger lesions and fibrotic changes.
Your ophthalmologist may suspect AMD if you are over 60 years of age and have recent changes in central vision. To establish a diagnosis a comprehensive eye checkup is done.
Visual Acuity test – This eye chart test measures how well you see at varying distances.
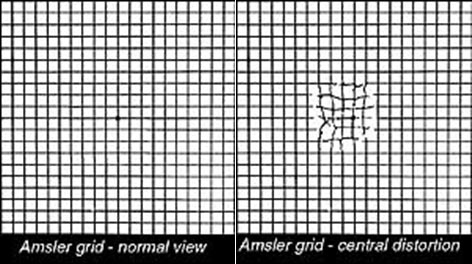
Amsler Grid – In this test the patient wearing his reading glasses, covers the opposite eye and looks at the black dot in the center of the test page (checkerboard pattern) to check for any area which is distorted, blurred, discolored or not visible. It is a useful test to detect early changes and can be done routinely by the patient at home.
Dilated eye examination – To look for signs of the disease your doctor will use drops to dilate or widen the pupil. With a special magnifying lens and a light source, your doctor will examine your retina. Dilating drops hamper close vision for around 4-5 hours.
If on the above examination your doctor suspects AMD, other tests to learn more about the structure and functioning of the retina could be advised.
Treatment Of Wet Age-Related Macular Degeneration
Wet AMD can be treated with laser photocoagulation, photodynamic therapy, intravitreal injections or a combination of these. The aim of treatment is to slow the rate of vision decrease or stop further vision loss but the disease sometimes may progress despite treatment. With the advent of anti-VEGF treatment, there are greater numbers of patients who are showing visual improvement.
Laser photocoagulation

This outpatient procedure uses the conventional laser to destroy fragile, leaking blood vessels. A high energy beam of light aimed directly at the new blood vessels, destroys and inactivates them, preventing further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue. Only a small percentage of patients where the membrane is away from the center (fovea) can be treated by this modality. Re-treatments may be necessary. Recently in some cases, we combine it with an anti-VEGF agent so as to decrease the chances of recurrence.
Photodynamic Therapy (PDT)
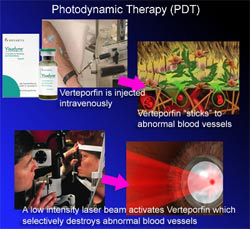
Photodynamic therapy (PDT) has been found to be an effective treatment for the patient for patients with new vessels (choroidal neovascular membrane or CNVM) secondary to AMD, myopia, etc. It reduces the risk of moderate and severe vision loss. A light stimulated drug called Verteporfin is injected intravenously. It travels throughout the body including the new vessels in the eye. The drug tends to “stick” to the surface of new blood vessels. Next, a low-intensity laser beam (689nm) is directed into the eye for about 83 seconds to activate the drug. The activated drug selectively destroys the abnormal blood vessels without damage to surrounding healthy tissue. Because the drug is activated by light the patient must avoid exposure to skin or eyes to direct sunlight or bright indoor light for 5 days after treatment. The treatment is relatively painless and no major side effects have been reported. PDT slows the rate of vision loss. Re-treatment may be required but usually not before 3 months.
Intravitreal Injections (Anti-VEGF Agents)
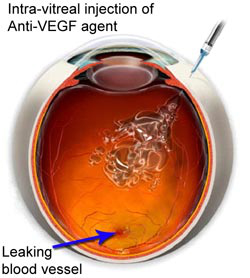
Abnormally high levels of Vascular Endothelial Growth Factor (VEGF) occur in eyes with wet AMD which promotes the growth of abnormal new blood vessels. Anti-VEGF agents block the effects of this growth factor. Treatment by this agent helps slow down vision loss from AMD and in some case improves vision. Multiple injections are often required for complete inactivation of the disease process.
Avastin (Bevacizumab) is an anti-VEGF agent approved for use in colorectal cancer. Ophthalmologists are using it “off-label” in AMD and other vascular conditions for its anti-angiogenic property. When used in the eye as an intravitreal injection its dose is miniscule and risk of adverse systemic reactions like gastrointestinal perforation, thrombo-embolic reactions, hypertension, and proteinuria is negligible. There are no formal clinical trials with Avastin but recent experience with this drug has been encouraging with most patients getting stabilized and some improvements.
Macugen (Pegaptanib Sodium) is the first selective VEGF inhibitor which the FDA approved to treat the pathologic process underlying all subtypes of neovascular AMD. In clinical studies, Macugen was given every 6 weeks for up to two years and was found to preserve visual acuity of all subtypes of neovascular AMD. Its advantage lies in its selective systemic inhibition of VEGF, thereby making it possible for use in patients with recent cardiac history.
Lucentis (Ranibizumab) is a recently FDA approved anti-VEGF agent that neutralizes all active forms of vascular endothelial growth factor. It is a recombinant homogenized monoclonal antibody. Clinical trials with Lucentis have shown not only stabilization but also the improvement in visual acuity. In the multicentre trial comparing effectivity of Lucentis to sham injection for minimally classic or occult CNVM, it was found that 94.5% of the group given 0.3 mg and 94.6 % of those given 0.5mg had stable vision compared with 62.2 % of those receiving the sham injection. Visual acuity improved in 24.8 % of the 0.3 mg group and 33.8% of 0.5 mg group as compared with 5% of the sham injection group. The benefit in visual acuity was maintained at 24 months. Lucentis was also found to be superior to Verteporfin (Photodynamic therapy) in predominantly classic neovascular age-related macular degeneration with low rates of serious ocular adverse effects.
Triamcinolone is a slow releasing steroid preparation which helps in reducing the swelling associated with the disease and also has some anti-angiogenic action. The risk of increased intraocular pressure is its major disadvantage. Since it is a suspension it is visible as a floater in the upper field of vision for a few weeks after injection.
Intravitreal injections are given with aseptic precautions in an operation theatre. The eye is numbed with anesthetic drops and then the injection is given. The procedure is relatively atraumatic but carries a small risk of post-injection infection, raised or low intraocular pressure, cataract formation, vitreous hemorrhage, retinal detachment. Systemically anti-VEGF agents are to be used with caution in patients with a recent history of cardiac ailment, uncontrolled hypertension, and severe proteinuria.
Combination Therapy
Treatment of wet ARMD with Photodynamic Therapy (PDT) alone has very limited chances of visual improvement while anti-VEGF agents have the problem associated with repeated injections. Combination therapy of PDT with anti-VEGF agents or Triamcinolone makes the treatment more finite, with the advantage of improvement in visual acuity in some cases and reduced requirement for repeated injections
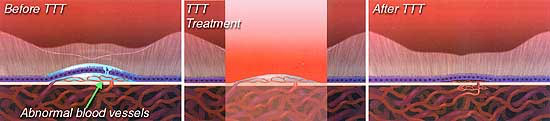
Transpupillary Thermotherapy (TTT)
In TTT, a large spot of diode laser (810 nm) with relatively low energy is applied to the area of new vessels. The treatment is non-specific and there is concomitant damage to normal retinal tissue though less than in conventional laser photocoagulation.
Surgical Treatment
The following surgical procedures have been tried but with limited benefit:
Excision of Subfoveal CNVM – The technique for this has been fairly well perfected but visual recovery is limited by the fact that normal retinal pigment epithelial cells are also removed in the process.
Macular Translocation – In this procedure, the retina is detached to be able to shift the fovea away from the subfoveal choroidal neovascular membrane. Thereafter the membrane is lasered without damaging the fovea. Drawbacks of this procedure are a high complication rate, the inadequate shift of macula, formation of retinal folds and double vision.
Treatment Of Dry Age-Related Macular Degeneration
There is no definite treatment for the dry form but the AREDS (Age-related Eye Disease Study) found that a specific high dose formation of antioxidants and zinc significantly reduces the risk of advanced AMD and its associated vision loss. Regular Amsler grid monitoring to detect conversion of dry form to wet form is important. Smokers should ensure that the formulation they take does not contain Beta-Carotene as that may increase their risk of developing lung cancer.
Yearly complete eye check up
Regular Amsler monitoring once the patient is diagnosed to have AMD.
Anti-oxidants to decrease progression of AMD.
A healthy diet rich in green leafy vegetables and fish.
Avoid smoking.
Maintain normal BP
Exercise and avoid obesity.
If you have lost sight from AMD do not be afraid to use your eyes for reading, watching TV.
Research
Scientists are studying the possibility of transplanting healthy cells into a diseased retina, and are evaluating families with a history of AMD to understand the genetic and hereditary factors that may cause the disease. They are also looking at certain anti-inflammatory treatments for the wet form of AMD.
This research should provide in the future, better ways to detect, treat and prevent vision loss in the patient with AMD.
Request a call back
I agree to recieve more information regarding services and offers at shroff eye center via SMS and Email
Disclaimer
This is not medical advice. Your ophthalmologist will help you decide which procedure and lens is best suited for your eyes. Every patient and eye is different and thus the experience for every patient is variable.
All product and company names are trademarks or registered trademarks of their respective holders. Use of them does not imply any affiliation or endorsement by them.

By being on the website, your personal data is being processed for communication with you and providing services. We use cookies to collect and analyse information on site performance, usage, enhancement of customer usability and improvising the website. We have put in place terms of use,
By clicking on accept you agree to all the policies mentioned above. You can read more about them by clicking on read more and accept them individually.








 Call us
Call us Email us
Email us


