Pediatric Opthalmology
Leaders in Eye care since 1914
NABH accredited

Zee healthcare leadership award
Awarded top eye centre
2016 & 2017
Awarded trusted eye centre
2017-18

#8 Eye Hospital in India*

#2 Eye Hospital in Delhi NCR*
FAQs
PATIENT TESTIMONIAL

What are the common eye problems in children?
Children can have a variety of eye problems
Other less common eye conditions in children are congenital glaucoma, corneal dystrophies, developmental abnormalities of the eyes (microphthalmos), subluxation of lens, persistent fetal vasculature syndrome (PHPV), chorioretinal coloboma, tumors (Retinoblastoma), albinism, aniridia and optic disc abnormalities (coloboma, hypoplasia, optic atrophy, swollen optic discs).
Children with systemic conditions like cerebral palsy and autism often have associated visual impairment. Some syndromic disorders like Marfan syndrome, Juvenile Idiopathic Arthritis and Osteogenesis imperfecta may also first present with eye complaints.
At Shroff Eye Centre, we are fully equipped to diagnose and manage these eye problems in children.
Our child eye specialists in Delhi NCR are leading authorities in eye problems in childhood.
How will I know my child has vision problems?

Repeated
watering of
eyes
Squeezing of
eyes
Frequent
rubbing of
eyes
Holding books
very near the eyes
or sitting close to
the TV to watch
Headaches
Abnormal
movements
of the eyes
In very young children, observation of delayed visual milestones, like not following bright lights, toys, faces,
should also prompt an early eye check up.
The deviation of eyes, nystagmus (to and fro movements of the eyes), abnormal head postures, roving eye movements
in children are often associated with amblyopia.
These conditions require an urgent consultation with child eye experts.

How early should an eye check up for a child be done ?
In the absence of any of the above problems, it is recommended that every child should have a routine eye check up at 3 years of age. Vision screening should be mandatory at the time of school admission. This should be followed by annual routine check ups.
Why should you choose Shroff eye centre for
your child’s eye care?
At Shroff Eye Centre, we have a dedicated Pediatric Ophthalmology and Strabismus Clinic in Delhi NCR.
Our goal is to reduce blindness in infants and children with eye disorders and help parents understand the problem.
Led by our top pediatric eye specialists, our team of specially trained staff uses child-friendly equipment to run amongst the best child eye clinics in India.
A separate child play-area, separate OPDs, Vision therapy clinic, portable slit lamps, portable non contact tonometry, orthoptic equipment, Synaptophore all available for the benefit of our pediatric patients at the clinic.
Our pediatric eye surgeons also perform procedures and surgeries in our advanced OT suites to ensure the best results.
Testimonials
Don’t just take our word.
Here’s what patients have to say!

Ms. Simonil jassawala
Madhav
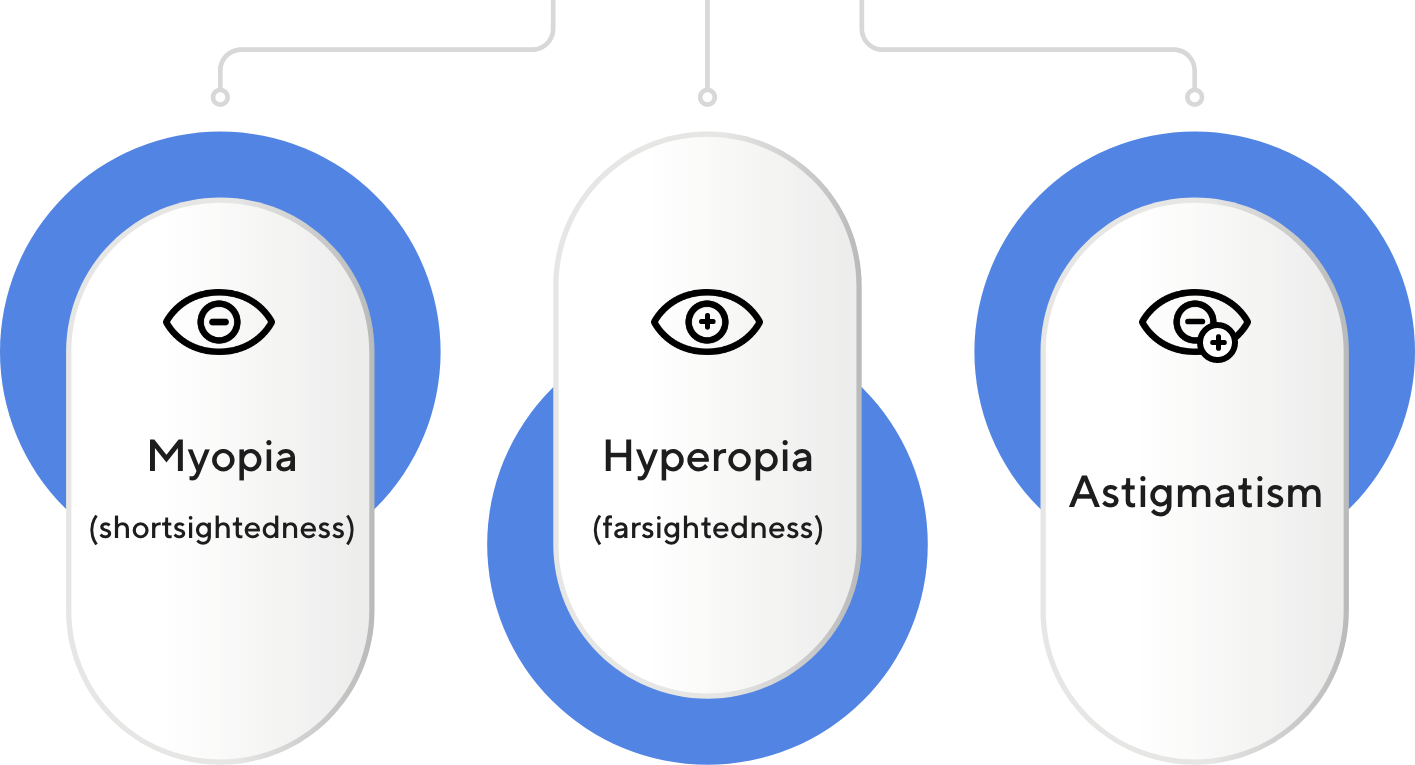
What are Refractive errors?
Refractive errors are disturbances in vision caused by the inability of light to focus on the retina.
Refractive errors are
Allergic Eye Disease

What are the common causes of Red Eye in children?
“Red Eye,” or conjunctivitis, is a non-specific
finding that simply indicates conjunctival
inflammation.
The most common causes for the pediatric pink
eye are allergic conjunctivitis, bacterial
conjunctivitis, viral conjunctivitis, and blepharitis
(inflammation of lid margins).
The vast majority of children who present with
“pink eye” will have simple conjunctivitis. Other
less common causes of a “red, teary eye” in
infants include congenital glaucoma and
nasolacrimal duct obstruction.
Consult with the top pediatric ophthalmologists in Gurgaon
Amblyopia
What is Amblyopia
(Lazy Eyes)?
Amblyopia or ‘Lazy Eyes’ is defined as binocular or monocular decrease in best corrected vision (even after spectacle correction), for which no apparent organic cause is found on eye examination. In simpler terms, it is the decrease in vision even after proper spectacles, in one or both eyes, which is not caused by any other eye problem or disease.
Squint
What is Strabismus? What is
squint or Deviation of eyes?
Misalignment of eyes is called strabismus, or squint,
and can lead to disruption of the visual development
process. It can occur in children or adults.
At Shroff Eye Centre, we provide consultation and
treatment for children and adults with squint (eye
muscle problems).
In the clinic, we approach each patient with special
attention and assess the problems for appropriate
diagnosis and treatment strategies.
Visit the best child eye specialists in Ghaziabad.
Cataract in childhood

What is a Cataract?
Cataracts occur when changes in the natural lens of
the eye cause it to become less transparent (clear).
This results in clouded or misty vision.
The lens is the transparent structure located just
behind the pupil (the black circle in the centre of the
eye). It allows light to reach the retina in the back of
the eye to allow image formation.
Other FAQs
-
How is cataract managed in children and what is its visual prognosis?
-
What are the Management options for Amblyopia?
-
How Amblyopia is commonly diagnosed?
-
What is Amblyopia (Lazy Eyes) and what are its important causes?
-
What are the latest advances in Intraocular Lens (IOL) technology?
-
What is Pseudo-strabismus?
-
How is strabismus surgery done, and what are the risks involved?
-
What are the common types of Strabismus and their management options?
-
What is Strabismus (Deviation of eyes)?
-
What is normal binocular vision?
-
What is a chalazion?
-
What are the common causes of Red Eye in children?
-
How early does my child need an eye check up?
-
What are the common eye problems seen in pediatric age group?
-
Pediatric Ophthalmology Service
-
What is the common cause of watering of eyes in infancy and how is it managed?
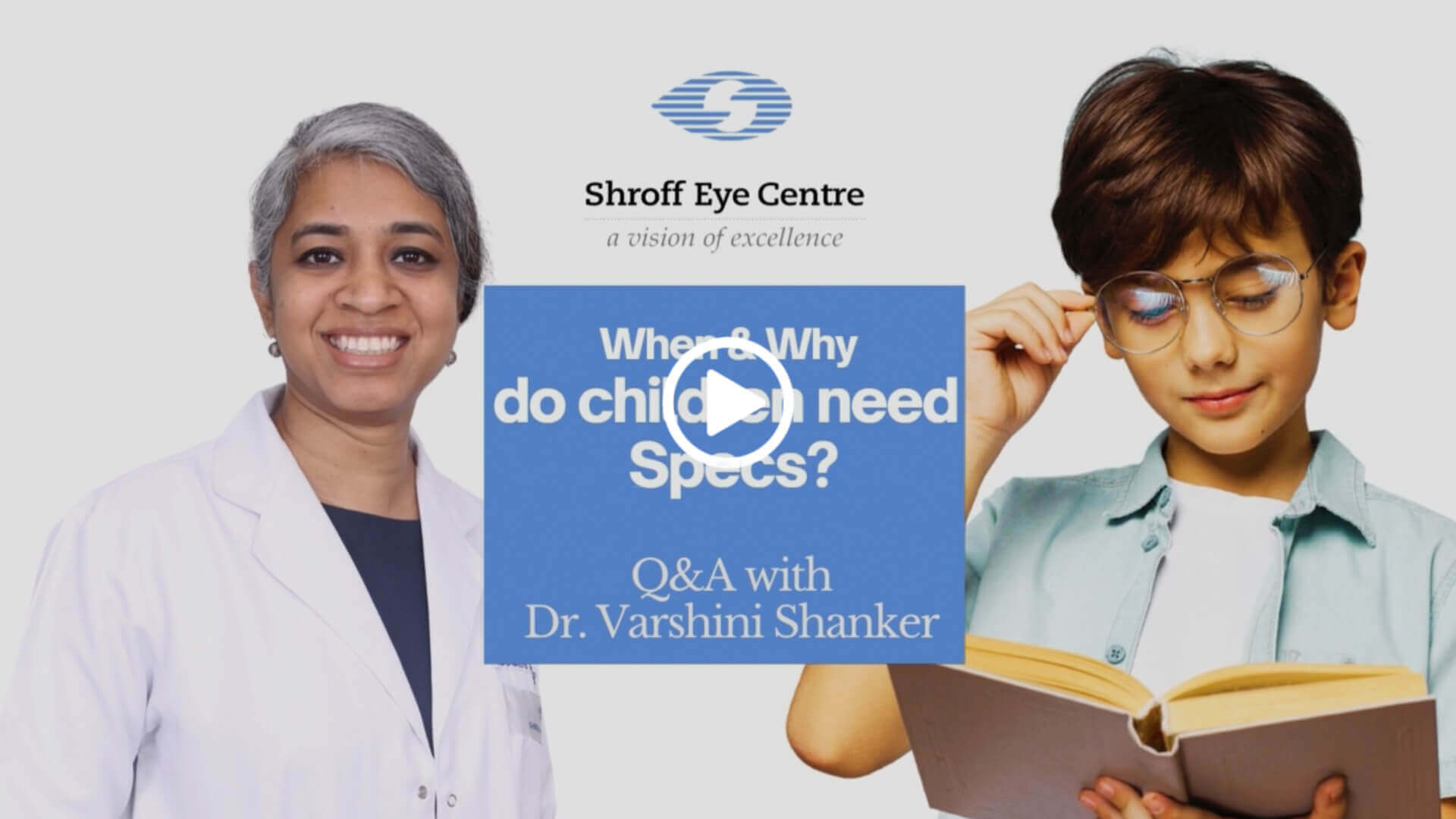
Our Team
Our leading Pediatric Ophthalmology experts in Delhi NCR
Our Locations
-
New Delhi
Kailash Colony
011 41633999A-9,
get directions
Kailash Colony,
New Delhi - 110 048 -
New Delhi
Connaught Place
011 41510906105 Surya Kiran, First floor
get directions
19, Kasturba Gandhi Marg,
New Delhi 110001 -
Haryana
Gurgaon
+91-124-4709999110, Bestech Chambers (Radisson Suites),
get directions
B Block, Sushant Lok Phase I, Sector 27,
Gurgaon, Haryana - 122002
-
Delhi NCR
Ghaziabad
+91 8826263999509, KM Trade Tower, Adjacent to Radisson blu , Sector 14, Kaushambi,
get directions
Ghaziabad, Uttar Pradesh -201010








 Call us
Call us Email us
Email us




 Call now
Call now